Abstract
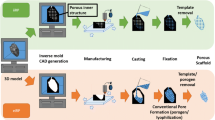
The incidence of bone disorders, whether due to trauma or pathology, has been trending upward with the aging of the worldwide population. The currently available treatments for bone injuries are rather limited, involving mainly bone grafts and implants. A particularly promising approach for bone regeneration uses rapid prototyping (RP) technologies to produce 3D scaffolds with highly controlled structure and orientation, based on computer-aided design models or medical data. Herein, tricalcium phosphate (TCP)/alginate scaffolds were produced using RP and subsequently their physicochemical, mechanical and biological properties were characterized. The results showed that 60/40 of TCP and alginate formulation was able to match the compression and present a similar Young modulus to that of trabecular bone while presenting an adequate biocompatibility. Moreover, the biomineralization ability, roughness and macro and microporosity of scaffolds allowed cell anchoring and proliferation at their surface, as well as cell migration to its interior, processes that are fundamental for osteointegration and bone regeneration.









Similar content being viewed by others
References
Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: an update. Injury. 2005;36(Suppl 3):S20–7. doi:10.1016/j.injury.2005.07.029.
O’Brien FJ. Biomaterials & scaffolds for tissue engineering. Mater Today. 2011;14(3):88–95. doi:10.1016/S1369-7021(11)70058-X.
Bobe K, Willbold E, Morgenthal I, Andersen O, Studnitzky T, Nellesen J, et al. In vitro and in vivo evaluation of biodegradable, open-porous scaffolds made of sintered magnesium W4 short fibres. Acta Biomater. 2013;9(10):8611–23.
Rai R, Keshavarz T, Roether JA, Boccaccini AR, Roy I. Medium chain length polyhydroxyalkanoates, promising new biomedical materials for the future. Mater Sci Eng, R. 2011;72(3):29–47.
He J, Huang T, Gan L, Zhou Z, Jiang B, Wu Y, et al. Collagen-infiltrated porous hydroxyapatite coating and its osteogenic properties: in vitro and in vivo study. J Biomed Mater Res Part A. 2012;100(A(7)):1706–15.
Chiara G, Letizia F, Lorenzo F, Edoardo S, Diego S, Stefano S, et al. Nanostructured biomaterials for tissue engineered bone tissue reconstruction. Int J Mol Sci. 2012;13(1):737–57.
Xie M, Olderøy MO, Zhang Z, Andreassen JP, Strand BL, Sikorski P. Biocomposites prepared by alkaline phosphatase mediated mineralization of alginate microbeads. RSC Adv. 2012;2(4):1457–65.
Wu S, Liu X, Yeung KWK, Hu T, Xu Z, Chung JCY, et al. Hydrogen release from titanium hydride in foaming of orthopedic NiTi scaffolds. Acta Biomater. 2011;7(3):1387–97.
Alvarez K, Nakajima H. Metallic Scaffolds for Bone Regeneration. Materials. 2009;2(3):790–832.
Li Z, Gu X, Lou S, Zheng Y. The development of binary Mg-Ca alloys for use as biodegradable materials within bone. Biomaterials. 2008;29(10):1329–44.
Wu S, Liu X, Yeung KW, Liu C, Yang X. Biomimetic porous scaffolds for bone tissue engineering. Mater Sci Eng. 2014;80:1–36.
Malda J, Visser J, Melchels FP, Jüngst T, Hennink WE, Dhert WJA, et al. 25th anniversary article: engineering hydrogels for biofabrication. Adv Mater. 2013;25(36):5011–28. doi:10.1002/adma.201302042.
Frohlich M, Grayson W, Wan L, Marolt D, Drobnic M, Vunjak- Novakovic G. Tissue engineered bone grafts: biological requirements, tissue culture and clinical relevance. Curr Stem Cell Res Ther. 2008;3(4):254–64. doi:10.2174/157488808786733962.
Gaalen SV, Kruyt M, Meijer G, Mistry A, Mikos A, Beucken JVD, et al. Tissue engineering of bone. In: Blitterswijk CV, Thomsen P, Lindahl A, Hubbell J, Williams DF, Cancedda R, et al., editors. Tissue engineering. Burlington: Academic Press; 2008. p. 559–610.
Bose S, Roy M, Bandyopadhyay A. Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 2012;30(10):546–54.
Ma PX. Biomimetic materials for tissue engineering. Adv Drug Deliv Rev. 2008;60(2):184–98. doi:10.1016/j.addr.2007.08.041.
Kneser U, Schaefer DJ, Polykandriotis E, Horch RE. Tissue engineering of bone: the reconstructive surgeon’s point of view. J Cell Mol Med. 2006;10(1):7–19. doi:10.1111/j.1582-4934.2006.tb00287.x.
Mikos AG, Bao Y, Cima LG, Ingber DE, Vacanti JP, Langer R. Preparation of poly(glycolic acid) bonded fiber structures for cell attachment and transplantation. J Biomed Mater Res. 1993;27(2):183–9. doi:10.1002/jbm.820270207.
Tuzlakoglu K, Bolgen N, Salgado AJ, Gomes ME, Piskin E, Reis RL. Nano- and micro-fiber combined scaffolds: a new architecture for bone tissue engineering. J Mater Sci. 2005;16(12):1099–104. doi:10.1007/s10856-005-4713-8.
Deville S, Saiz E, Tomsia AP. Freeze casting of hydroxyapatite scaffolds for bone tissue engineering. Biomaterials. 2006;27(32):5480–9. doi:10.1016/j.biomaterials.2006.06.028.
Kim H-W, Knowles JC, Kim H-E. Hydroxyapatite and gelatin composite foams processed via novel freeze-drying and crosslinking for use as temporary hard tissue scaffolds. J Biomed Mater Res, Part A. 2005;72A(2):136–45. doi:10.1002/jbm.a.30168.
Gomes ME, Ribeiro AS, Malafaya PB, Reis RL, Cunha AM. A new approach based on injection moulding to produce biodegradable starch-based polymeric scaffolds: morphology, mechanical and degradation behaviour. Biomaterials. 2001;22(9):883–9. doi:10.1016/S0142-9612(00)00211-8.
Mondrinos MJ, Dembzynski R, Lu L, Byrapogu VKC, Wootton DM, Lelkes PI, et al. Porogen-based solid freeform fabrication of polycaprolactone–calcium phosphate scaffolds for tissue engineering. Biomaterials. 2006;27(25):4399–408. doi:10.1016/j.biomaterials.2006.03.049.
Duarte ARC, Mano JF, Reis RL. Dexamethasone-loaded scaffolds prepared by supercritical-assisted phase inversion. Acta Biomater. 2009;5(6):2054–62. doi:10.1016/j.actbio.2009.01.047.
Tsivintzelis I, Pavlidou E, Panayiotou C. Porous scaffolds prepared by phase inversion using supercritical CO2 as antisolvent: i. Poly(l-lactic acid). J Supercrit Fluids. 2007;40(2):317–22. doi:10.1016/j.supflu.2006.06.001.
Suh SW, Shin JY, Kim J, Kim J, Beak CH, Kim DI, et al. Effect of different particles on cell proliferation in polymer scaffolds using a solvent-casting and particulate leaching technique. ASAIO J. 2002;48(5):460–4.
Sin D, Miao X, Liu G, Wei F, Chadwick G, Yan C, et al. Polyurethane (PU) scaffolds prepared by solvent casting/particulate leaching (SCPL) combined with centrifugation. Mater Sci Eng C. 2010;30(1):78–85. doi:10.1016/j.msec.2009.09.002.
Salgado AJ, Coutinho OP, Reis RL. Bone tissue engineering: state of the art and future trends. Macromol Biosci. 2004;4(8):743–65. doi:10.1002/mabi.200400026.
Daniel LC, Jeffrey IL, Lawrence JB, Hod L. Additive manufacturing for in situ repair of osteochondral defects. Biofabrication. 2010;2(3):035004.
Malone E, Lipson H. Fab@Home: the personal desktop fabricator kit. Rapid Prototyp J. 2007;13(4):245–55. doi:10.1108/13552540710776197.
Fedorovich NE, Schuurman W, Wijnberg HM, Prins H-J, van Weeren PR, Malda J, et al. Biofabrication of osteochondral tissue equivalents by printing topologically defined, cell-laden hydrogel scaffolds. Tissue Eng Part C. 2011;18(1):33–44. doi:10.1089/ten.tec.2011.0060.
Shaffer S, Yang K, Vargas J, Di Prima MA, Voit W. On reducing anisotropy in 3D printed polymers via ionizing radiation. Polymer. 2014;55(23):5969–79.
Martínez-Vázquez FJ, Perera FH, Miranda P, Pajares A, Guiberteau F. Improving the compressive strength of bioceramic robocast scaffolds by polymer infiltration. Acta Biomater. 2010;6(11):4361–8. doi:10.1016/j.actbio.2010.05.024.
Hockaday LA, Kang KH, Colangelo NW, Cheung PYC, Duan B, Malone E, et al. Rapid 3D printing of anatomically accurate and mechanically heterogeneous aortic valve hydrogel scaffolds. Biofabrication. 2012;4(3):035005.
Santos CFL, Silva AP, Lopes L, Pires I, Correia IJ. Design and production of sintered β-tricalcium phosphate 3D scaffolds for bone tissue regeneration. Mater Sci Eng. 2012;32(5):1293–8. doi:10.1016/j.msec.2012.04.010.
Diogo GS, Gaspar VM, Serra IR, Fradique R, Correia IJ. Manufacture of β-TCP/alginate scaffolds through a Fab@home model for application in bone tissue engineering. Biofabrication. 2014;6(2):025001. doi:10.1088/1758-5082/6/2/025001.
Kang KH, Hockaday LA, Butcher JT. Quantitative optimization of solid freeform deposition of aqueous hydrogels. Biofabrication. 2013;5(3):035001.
Rezwan K, Chen QZ, Blaker JJ, Boccaccini AR. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials. 2006;27(18):3413–31. doi:10.1016/j.biomaterials.2006.01.039.
Choi D, Kumta PN. Mechano-chemical synthesis and characterization of nanostructured β-TCP powder. Mater Sci Eng C. 2007;27(3):377–81. doi:10.1016/j.msec.2006.05.035.
Andersen T, Strand BL, Formo K, Alsberg E, Christensen BE. Chapter 9 Alginates as biomaterials in tissue engineering. Carbohydrate chemistry, vol. 37. Cambridge: The Royal Society of Chemistry; 2012. p. 227–58.
Augst AD, Kong HJ, Mooney DJ. Alginate hydrogels as biomaterials. Macromol Biosci. 2006;6(8):623–33. doi:10.1002/mabi.200600069.
Bonino CA, Krebs MD, Saquing CD, Jeong SI, Shearer KL, Alsberg E, et al. Electrospinning alginate-based nanofibers: from blends to crosslinked low molecular weight alginate-only systems. Carbohydr Polym. 2011;85(1):111–9. doi:10.1016/j.carbpol.2011.02.002.
Valente JFA, Valente TAM, Alves P, Ferreira P, Silva A, Correia IJ. Alginate based scaffolds for bone tissue engineering. Mater Sci Eng C. 2012;32(8):2596–603. doi:10.1016/j.msec.2012.08.001.
Lima AC, Batista P, Valente TA, Silva AS, Correia IJ, Mano JF. Novel methodology based on biomimetic superhydrophobic substrates to immobilize cells and proteins in hydrogel spheres for applications in bone regeneration. Tissue Eng Part A. 2013;19(9–10):1175–87.
Li Z, Ramay HR, Hauch KD, Xiao D, Zhang M. Chitosan–alginate hybrid scaffolds for bone tissue engineering. Biomaterials. 2005;26(18):3919–28. doi:10.1016/j.biomaterials.2004.09.062.
Lin H-R, Yeh Y-J. Porous alginate/hydroxyapatite composite scaffolds for bone tissue engineering: preparation, characterization, and in vitro studies. J Biomed Mater Res, Part B. 2004;71B(1):52–65. doi:10.1002/jbm.b.30065.
Yang F, Xia S, Tan C, Zhang X. Preparation and evaluation of chitosan-calcium-gellan gum beads for controlled release of protein. Eur Food Res Technol. 2013;237(4):467–79. doi:10.1007/s00217-013-2021-y.
Torres AL, Gaspar VM, Serra IR, Diogo GS, Fradique R, Silva AP, et al. Bioactive polymeric–ceramic hybrid 3D scaffold for application in bone tissue regeneration. Mater Sci Eng C. 2013;33(7):4460–9. doi:10.1016/j.msec.2013.07.003.
Jiankang H, Dichen L, Yaxiong L, Bo Y, Bingheng L, Qin L. Fabrication and characterization of chitosan/gelatin porous scaffolds with predefined internal microstructures. Polymer. 2007;48(15):4578–88. doi:10.1016/j.polymer.2007.05.048.
Jeong SI, Jeon O, Krebs MD, Hill MC, Alsberg E. Biodegradable photo-crosslinked alginate nanofibre scaffolds with tuneable physical properties, cell adhesivity and growth factor release. Eur cells Mater. 2012;24:331–43.
Freed LE, Vunjak-Novakovic G, Biron RJ, Eagles DB, Lesnoy DC, Barlow SK, et al. Biodegradable polymer scaffolds for tissue engineering. Nat Biotechnol. 1994;12(7):689–93.
Kokubo T, Takadama H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials. 2006;27(15):2907–15. doi:10.1016/j.biomaterials.2006.01.017.
Jalota S, Bhaduri SB, Tas AC. Using a synthetic body fluid (SBF) solution of 27 mM HCO3 − to make bone substitutes more osteointegrative. Mater Sci Eng C. 2008;28(1):129–40. doi:10.1016/j.msec.2007.10.058.
Lee JTY, Chow KL. SEM sample preparation for cells on 3D scaffolds by freeze-drying and HMDS. Scanning. 2012;34(1):12–25. doi:10.1002/sca.20271.
Schieker M, Seitz H, Drosse I, Seitz S, Mutschler W. Biomaterials as scaffold for bone tissue engineering. Eur J Trauma. 2006;32(2):114–24. doi:10.1007/s00068-006-6047-8.
Lawson MA, Barralet JE, Wang L, Shelton RM, Triffitt JT. Adhesion and growth of bone marrow stromal cells on modified alginate hydrogels. Tissue Eng. 2004;10(9–10):1480–91. doi:10.1089/ten.2004.10.1480.
Dittrich R, Tomandl G, Despang F, Bernhardt A, Hanke T, Pompe W, et al. Scaffolds for hard tissue engineering by ionotropic gelation of alginate-influence of selected preparation parameters. J Am Ceram Soc. 2007;90(6):1703–8. doi:10.1111/j.1551-2916.2007.01598.x.
Rassis DK, Saguy IS, Nussinovitch A. Collapse, shrinkage and structural changes in dried alginate gels containing fillers. Food Hydrocoll. 2002;16(2):139–51. doi:10.1016/S0268-005X(01)00071-6.
Deligianni DD, Katsala ND, Koutsoukos PG, Missirlis YF. Effect of surface roughness of hydroxyapatite on human bone marrow cell adhesion, proliferation, differentiation and detachment strength. Biomaterials. 2000;22(1):87–96. doi:10.1016/S0142-9612(00)00174-5.
Rechendorff K, Hovgaard MB, Foss M, Zhdanov VP, Besenbacher F. Enhancement of protein adsorption induced by surface roughness. Langmuir. 2006;22(26):10885–8. doi:10.1021/la0621923.
Lawrie G, Keen I, Drew B, Chandler-Temple A, Rintoul L, Fredericks P, et al. Interactions between Alginate and chitosan biopolymers characterized using FTIR and XPS. Biomacromolecules. 2007;8(8):2533–41. doi:10.1021/bm070014y.
Daemi H, Barikani M. Synthesis and characterization of calcium alginate nanoparticles, sodium homopolymannuronate salt and its calcium nanoparticles. Sci Iran. 2012;19(6):2023–8. doi:10.1016/j.scient.2012.10.005.
Tzaphlidou M, Zaichick V. Calcium, Phosphorus, calcium-phosphorus ratio in rib bone of healthy humans. Biol Trace Elem Res. 2003;93(1–3):63–74. doi:10.1385/BTER:93:1-3:63.
Mansur HS, Costa HS. Nanostructured poly(vinyl alcohol)/bioactive glass and poly(vinyl alcohol)/chitosan/bioactive glass hybrid scaffolds for biomedical applications. Chem Eng J. 2008;137(1):72–83. doi:10.1016/j.cej.2007.09.036.
Wei G, Ma PX. Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials. 2004;25(19):4749–57. doi:10.1016/j.biomaterials.2003.12.005.
Román J, Cabañas MV, Peña J, Doadrio JC, Vallet-Regí M. An optimized β-tricalcium phosphate and agarose scaffold fabrication technique. J Biomed Mater Res, Part A. 2008;84A(1):99–107. doi:10.1002/jbm.a.31394.
Shi L, Shi L, Wang L, Duan Y, Lei W, Wang Z, et al. The improved biological performance of a novel low elastic modulus implant. PLoS ONE. 2013;8(2):e55015. doi:10.1371/journal.pone.0055015.
Tam SK, Dusseault J, Bilodeau S, Langlois G, Hallé J-P, Yahia LH. Factors influencing alginate gel biocompatibility. J Biomed Mater Res, Part A. 2011;98A(1):40–52. doi:10.1002/jbm.a.33047.
Hu Y, Wang J, Xing W, Cao L, Liu C. Surface-modified pliable PDLLA/PCL/β-TCP scaffolds as a promising delivery system for bone regeneration. J Appl Polym Sci. 2014;. doi:10.1002/app.40951.
Dowling DP, Miller IS, Ardhaoui M, Gallagher WM. Effect of surface wettability and topography on the adhesion of osteosarcoma cells on plasma-modified polystyrene. J Biomater Appl. 2011;26(3):327–47. doi:10.1177/0885328210372148.
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26(27):5474–91. doi:10.1016/j.biomaterials.2005.02.002.
Renders GAP, Mulder L, Van Ruijven LJ, Van Eijden TMGJ. Porosity of human mandibular condylar bone. J Anat. 2007;210(3):239–48. doi:10.1111/j.1469-7580.2007.00693.x.
Dumas JE, Prieto EM, Zienkiewicz KJ, Guda T, Wenke JC, Bible J, et al. Balancing the rates of new bone formation and polymer degradation enhances healing of weight-bearing allograft/polyurethane composites in rabbit femoral defects. Tissue Eng Part A. 2014;20(1–2):115–29. doi:10.1089/ten.TEA.2012.0762.
Kamitakahara M, Ohtsuki C, Miyazaki T. Review paper: behavior of ceramic biomaterials derived from tricalcium phosphate in physiological condition. J Biomater Appl. 2008;23(3):197–212. doi:10.1177/0885328208096798.
Franco J, Hunger P, Launey ME, Tomsia AP, Saiz E. Direct write assembly of calcium phosphate scaffolds using a water-based hydrogel. Acta Biomater. 2010;6(1):218–28. doi:10.1016/j.actbio.2009.06.031.
Yin Y, Ye F, Cui J, Zhang F, Li X, Yao K. Preparation and characterization of macroporous chitosan–gelatin/β-tricalcium phosphate composite scaffolds for bone tissue engineering. J Biomed Mater Res, Part A. 2003;67A(3):844–55. doi:10.1002/jbm.a.10153.
Acknowledgments
Authors would like to acknowledge funding from FEDER (POCI-COMPETE 2020, project number 007491), Portuguese Science Foundation (FCT) (UID/Multi/00709) and QREN (Programa Mais Centro) (CENTRO-07-0224-FEDER-002014).
Author information
Authors and Affiliations
Corresponding author
Additional information
R. Fradique and T. R. Correia have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10856_2016_5681_MOESM1_ESM.tif
Optical images of human osteoblast cells seeded in the presence of the different materials after 4 and 7 days of incubation at a magnification of 100×. Supplementary material 1 (TIFF 5088 kb)
Rights and permissions
About this article
Cite this article
Fradique, R., Correia, T.R., Miguel, S.P. et al. Production of new 3D scaffolds for bone tissue regeneration by rapid prototyping. J Mater Sci: Mater Med 27, 69 (2016). https://doi.org/10.1007/s10856-016-5681-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5681-x